Do you know the true history of women’s health research? How about its negative impact on the lives of women everywhere?
If not, it’s time for a mini history lesson!
For a history that has deep roots in sexism, racism, and classism, it isn’t always the most joyous of histories to share…
Although it’s a history that can be challenging to learn about, if we aren’t facing the problem at hand, I’m afraid nothing’s ever going to change.
Acknowledgements:
Before I dive into today’s history lesson, I want to acknowledge some of the pioneers in this work. Barbara Ehrenreich, Deirdre English, Deirdre Cooper Owens, Theo Colborn, Martie Haselton, Dr. Jerilynn Prior, and Maya Dusenbery. These are just a few to name that have been integral resources to my understanding of this topic.
Through their research, books, articles, and interviews, I have gleaned so much insight into just how dysfunctional these systems are. Unfortunately, bad medicine and flawed research have created a war against women for centuries.
How about we start from the beginning?
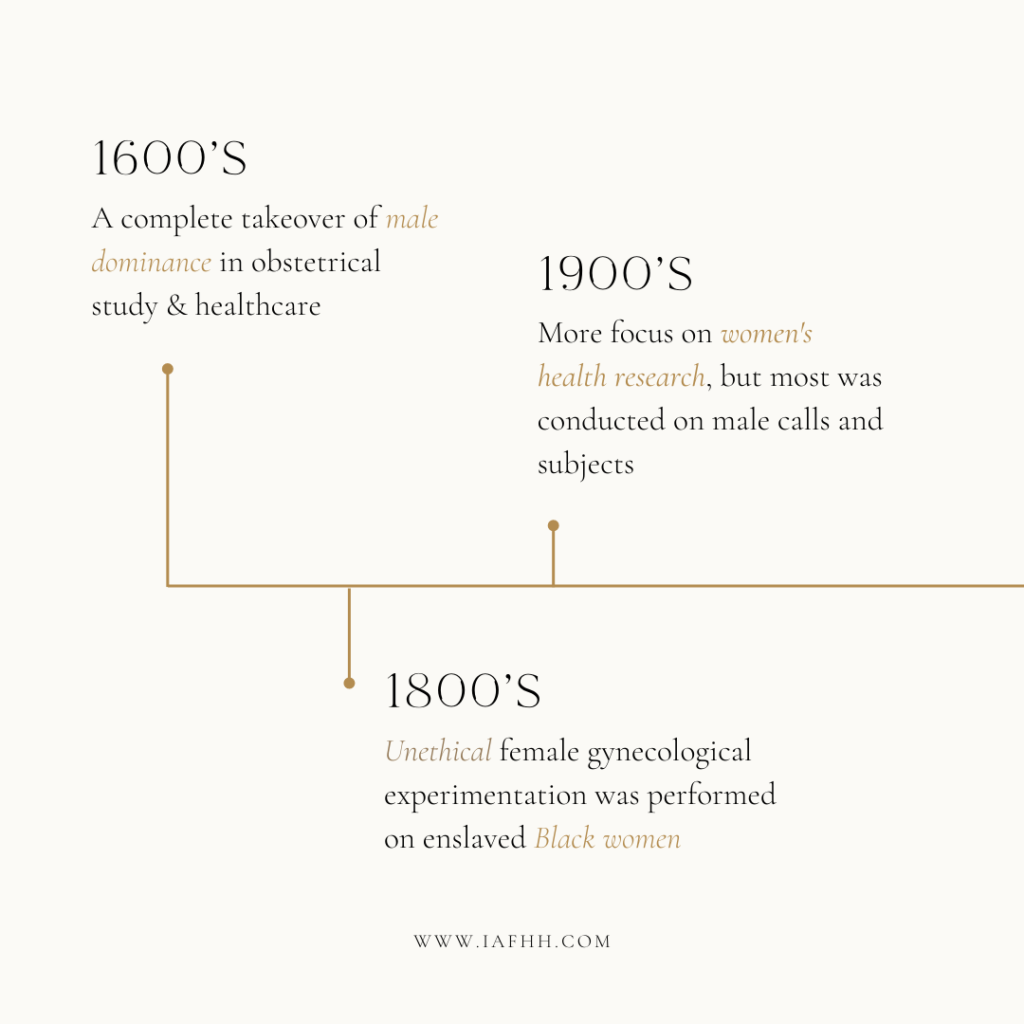
Women’s Health Research in the 1600s
Leading up to the 17th century, the age of witch-hunting was widespread. At the time, it was thought that women were practicing witchcraft if they took a part in any form of medicine, herbalism, or midwifery.
Over time, this led to the mass decimation of generational wisdom and knowledge pertaining to natural medicine. This required men to create their own systems and approaches to “medicine”, leaving women vulnerable to their naivety.
The Restrictive Nature of Male-Dominated Medicine
During this era, there were restrictions in place preventing women from having any role in health, medicine, and even birth. This turned into a complete takeover of male dominance in obstetrical study and healthcare come the 1600s.
A quote from the book ‘Witches, Midwives, and Nurses’ states:
“It was witches who developed an extensive understanding of bones and muscles, herbs and drugs, while physicians were still deriving their prognoses from astrology and alchemists were trying to turn lead into gold.”
Ehrenreich, B., & English, D. (2016). Witches, midwives, and nurses: A history of women healers. Last Work Press.
Overtime this led to an overhaul of male dominance in medicine and women’s health research. Unfortunately, it also created a dysfunctional foundation that still, even to this day, influences many of our modern healthcare practices.
Women’s Health Research in the 1800s
Come the 19th century, women’s health research took a turn for the worse. The “Father of Modern Gynecology”, Dr. James Marion Sims, routinely experimented with his gynecological research on enslaved Black women he leased for that very purpose. He also often performed his experiments without pain relief or medication, making this part of women’s health research quite disturbing. Unfortunately, many of the gynecological procedures that are used today have been influenced by this disturbing past.
You can read more about the grotesque history of modern gynecology in the book ‘Medical Bondage’, written by Deirdre Cooper Owens.
Women’s Health Research in the 1900s
Come the 1900s, women’s health and research started to expand, but not necessarily in the ways you may imagine…
During this time, more clinical research began to take place in controlled laboratory settings. However, many flaws within the conduction and analyzation have contributed the misinformation we have today regarding women’s health research.
Outside of the difference in sexual organs and monthly hormonal fluctuations, women were perceived to be physiologically equivalent to men. (Even though further, more privately funded research suggested otherwise!)
Today, a large majority of the research we have about the human body, including women’s health experiences, is conducted primarily on male cells and subjects.
The Inclusion of Women in Research:
In most cases, women were brought into clinical research only when it applied specifically to female experiences, such as pregnancy, or menopause. Although, there are still many questions with how research was conducted. For example, research may not consider important factors, such as a woman’s cyclical status, or whether or not she’s on hormonal birth control. In addition, research that did include women favored the inclusion of White women and left out many women of color and minorities.
Beyond this, female experiences aren’t as actively researched. This is especially true for conditions like PMS, PMDD, Vaginismus, Vulvodynia, Fibromyalgia, Multiple Sclerosis, POTS, and Chronic Fatigue Syndrome. More often, these conditions tend to be written off as a form of “Hysteria” or “Psychosomaticism”, if not disregarded entirely.
Leaning further into the 1900s, things started to improve, but not without their own set of pitfalls…
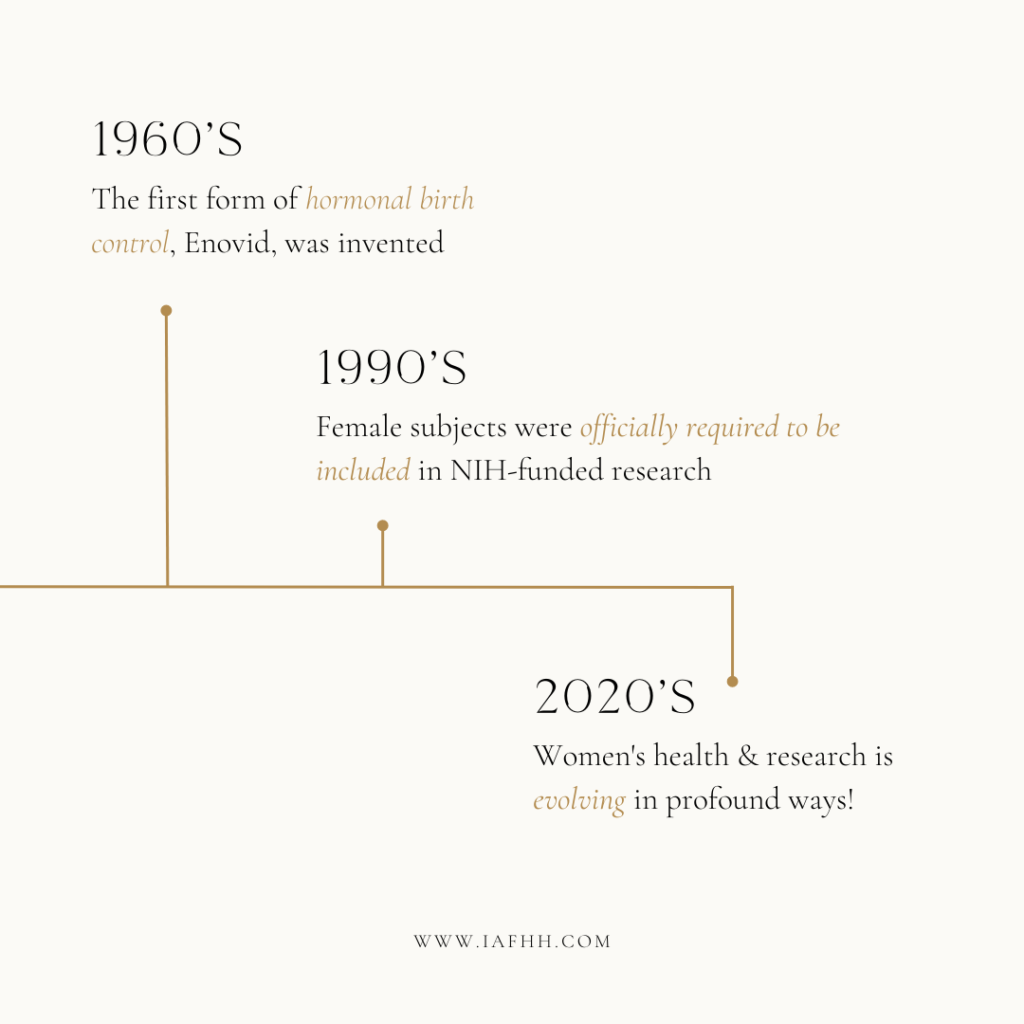
Women’s Health Research in the 1960s
Come the 1960s, the feminist revolution began to take place and had a huge impact on women’s reproductive freedom. Before this time, many women relied upon barrier methods, withdrawal, and spermicides for contraception. Meanwhile, they waited patiently for the invention of a “magic pill” that would make them less fertile.
Although the history of how the pill came to fruition is based upon a past of feminism and reproductive freedom, over time its usage has only led to further oppression of women’s reproductive health and rights.
The Invention of Enovid:
The first birth control pill, Enovid, was created through a mixture of synthetic hormones similar to natural progesterone and estrogen. They found that introducing these synthetic hormones suppressed natural hormone production resulting in temporary infertility. Its invention ultimately sparked feminist conversation around women’s reproductive rights and body autonomy. This gave women the opportunity to be freely in control of their reproductive choices. Talk about a huge step in the evolution of feminism!
However, what we know, and perhaps fail to admit on a larger scale, is that contraception from hormonal birth control can only happen at a great cost. The potential side effects of hormonal birth control is not a small list. Symptoms can range anywhere from depression to decreased libido to reproductive damage and infertility.
Fortunately, there are more alternatives available today that are healthier and more accessible for the average woman. These options are also supportive of female hormonal health instead of being suppressive. Sadly, dismissal of the advocacy for these alternatives is quite prevalent.
Women’s Health Research in the 1990s
Come the 1990s, we started to notice the downfalls of not regularly including women and minorities in research.
In 1993, the National Institutes of Health published the NIH Revitalization Act. This guideline states that funded clinical trials are required to include female subjects and minorities in their research.
Flaws With the NIH Revitalization Act
Although this may sound like a massive improvement and a huge leap toward more inclusive research, this regulation only applied to NIH-funded research. Meaning privately funded research was still exempt from this policy.
Beyond that, this policy only requires the inclusion of female subjects within Phase 3 human-based trials. It did not specify the inclusion within subclinical research. This leaves any research conducted on cells and animal subjects still largely male-oriented.
Phase 3 trials did initiate the inclusion of more female subjects. However, these guidelines do not require researchers to report their findings by sex. Unfortunately, this only leaves room for misinterpretation, inaccurate findings, and missing information.
Thankfully, over the past decade, there has been an improvement on this last piece. A quote from Maya Dusenbery’s book, ‘Doing Harm’ states:
“Today, according to Stanford University’s Gendered Innovations project, thirty-two peer-reviewed journals worldwide have editorial policies requiring that researchers include information on results by gender/sex when they submit articles for publication”.
Dusenbery, M. (2019). Doing harm. HarperOne.
However, it’s important to note that this wasn’t in place until about 2010.
Women’s Health Research in 2020s and beyond
Today, we are hopefully heading in a more positive direction! As we begin to point out these flaws and conduct more thorough research on women, my hope is that we continue to see improvements.
One of the most challenging aspects of this is that many medical schools are still teaching outdated information. In addition, conventional practitioners are continuing to perpetuate practices that are harmful to women. Such as contributing to forms of medical gaslighting and obstetric violence.
Today, we have more data than ever before on health inequities from women all over the world. This makes the work we do all the more essential to revolutionizing women’s health not just in the US, but all over the globe.
What We Can Do
As women’s health practitioners, it’s important we are aware of the dysfunctional history that has led to our modern-day understanding of women’s health.
The evolution of women’s health research and education is so incredibly dysfunctional, we cannot ignore it any longer.
It’s time re-evaluate how we’ve been working with women over the centuries, and lean into the evolving research we have available to us.
If we truly want to instill change in how women receive healthcare and support in this world, we need to realign our approaches to better include, consider, and support women on all levels.
This is the work we are dedicating ourselves to here at The International Association for Functional Hormone Health. This is what this community is for!
How You Can Get Involved
Not only are we spreading awareness about the flaws in research and medical practice that are harming women all over the world, but we are taking action by building community, expanding our resources, and deepening our knowledge in this area.
Here at IAFHH, our mission is to empower women’s health professionals with mastery of functional hormone health. We believe that collectively, we can transform how women and female bodies receive healthcare globally.
Through quality education, high-level mentorship, and community engagement, we are creating a new generation of women’s health practitioners that are dedicated to the innovation of women’s healthcare practices.
Learn more about our Functional Hormone Specialist Certification Program
Receive mentorship from one of our IAFHH advanced practitioners
Donate to our scholarship fund

About the Author
Ashe Milkovic, NTP, IC-FHS, FBCS
Ashe is the founder and CEO of The International Association for Functional Hormone Health. She has a passion for spreading awareness about the power of functional nutrition for optimizing hormones & fertility, and her mission is to build community and safe space for other practitioners and aspiring learners to expand their knowledge and expertise in functional hormone health.
