Are you interested in learning more about how hormones and the menstrual cycle influence women’s health but don’t find yourself as intrigued by the “fertility” side of things?
Perhaps your vision isn’t to support your clients in preparing for or achieving pregnancy, but rather, to help them overcome hormone imbalances such as PCOS or endometriosis, or to simply help them achieve more strength and vitality in their lives.
If so, I get it. Women’s health is so much more than female fecundity, and that deserves to be recognized and supported just as much as those who are fertility-focused.
However, one of the reasons why women haven’t been adequately supported in all areas of their lives is because of insufficient education on the importance of functional hormone health beyond reproductive function. Instead, many tend to believe that fertility is separate from hormone health. When in truth, they are two sides of the very same coin.
This article is going to shine a light on the connection between hormone health and fertility that you might not have recognized before, and will help you to understand why fertility matters in your female-focused practice, even if you aren’t a “fertility specialist”.

Why Fertility Matters
If your clients face cyclical symptoms such as period cramps, PMS, breast tenderness, or hormonal acne, they are likely experiencing some form of hormone imbalance. Similarly, fertility issues can often result from the same kinds of hormone imbalances.
Estrogen excess/dominance, low estrogen, low progesterone, high androgens, high prolactin, and low thyroid hormone are just a few hormone imbalances to note that may have an impact on both menstrual and fertility health outcomes.
The Impact of Hormone Imbalances
Imbalances in these essential hormones may impair fertility by causing an improper build-up and receptivity of the endometrial lining, the formation of abnormal growths such as cysts, fibroids, or endometrial lesions, as well as increased inflammation, immune and autoimmunity disorders, metabolic dysregulation, and/or anovulation — the lack of ovulation entirely. (1), (2), (3), (4)
However, the impact these imbalances can have does not stop at impairing one’s ability to conceive and reproduce. These imbalances can also result in symptoms such as increased PMS, mood swings, irritability, low libido, sleep disorders, digestive issues, increased pain/inflammation, decreased insulin sensitivity, impaired pelvic floor function, painful intercourse, low libido, hair loss/thinning, skin disturbances, and more.
When evaluating the extent of symptoms that hormone imbalances can cause, limiting the issue just to impairing one’s ability to reproduce is such a tunnel-vision perspective. Not only can these imbalances lead to various fertility complications, but perhaps more importantly, they can decrease a woman’s overall quality of life.
This is just an overview perspective of why fertility matters outside of fecundity, but let’s take this conversation a step further to understand the science behind how these imbalances contribute to these symptoms, and why fertility matters beyond baby-making.

Why Ovulation Matters
When evaluating our female client’s hormone health and fertility, we first need to consider their ovulatory function – that is, how, when, and if they are ovulating.
Why is ovulation so important?
During the follicular phase (before ovulation), the steroid hormone estrogen rises. Although estrogen is often villainized when it comes to hormone health, when in appropriate amounts estrogen has many health benefits.
For example, healthy estrogen levels in the follicular phase contribute to the growth and development of ovarian follicles, the production of fertile-quality cervical mucus, facilitates vaginal tissue health and repair, serotonin/dopamine production, insulin sensitivity, and more.
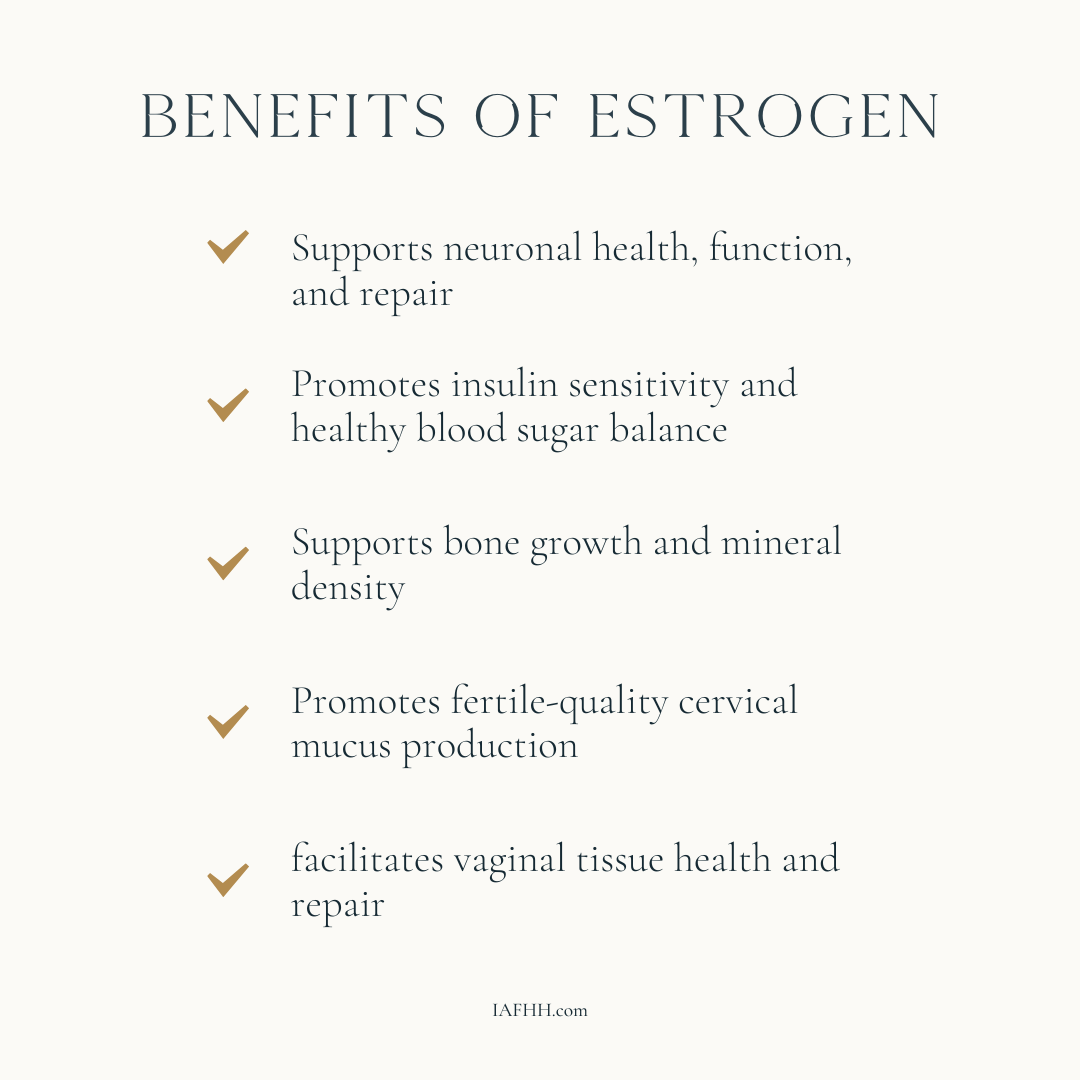
Benefits of estrogen:
- Healthy levels of estrogen support the health and function of the brain by increasing cerebral blood flow, increasing levels of the neurotransmitters Serotonin and Dopamine, and protecting against oxidative damage to the brain by stimulating the growth & repair of neurons. (5)
- Healthy levels of estrogen increase insulin sensitivity which can have a positive effect on blood sugar stability, improving glucose metabolism and modulating inflammation levels within the body. This in turn can support a healthy metabolism and weight maintenance. (6)
- Healthy levels of estrogen support bone health and density by enhancing calcium absorption into the bone, inhibiting bone resorption, and promoting bone-building activity. (7),(8)
After ovulation, the ovarian follicle that the egg ovulated from turns into the corpus luteum, a temporary endocrine gland that produces the steroid hormone, progesterone. (See image 1)
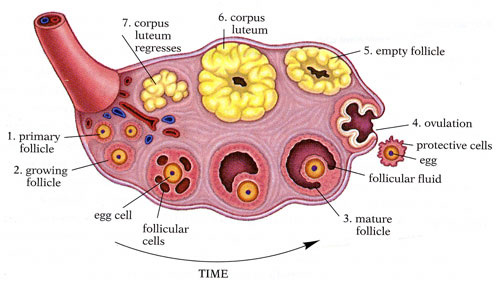
Image 1 – View of the ovarian cycle from follicle development to corpus luteum formation and regression
Image Source
Progesterone is considered a feel-good hormone, as it tends to have a sedative effect on the nervous system and brain, causing one to feel happier, more content, and sleepy during their luteal phase – the second half of their menstrual cycle. (In some cases, progesterone may lead to worsening symptoms, such as with PMDD, but that’s a conversation for another day!)
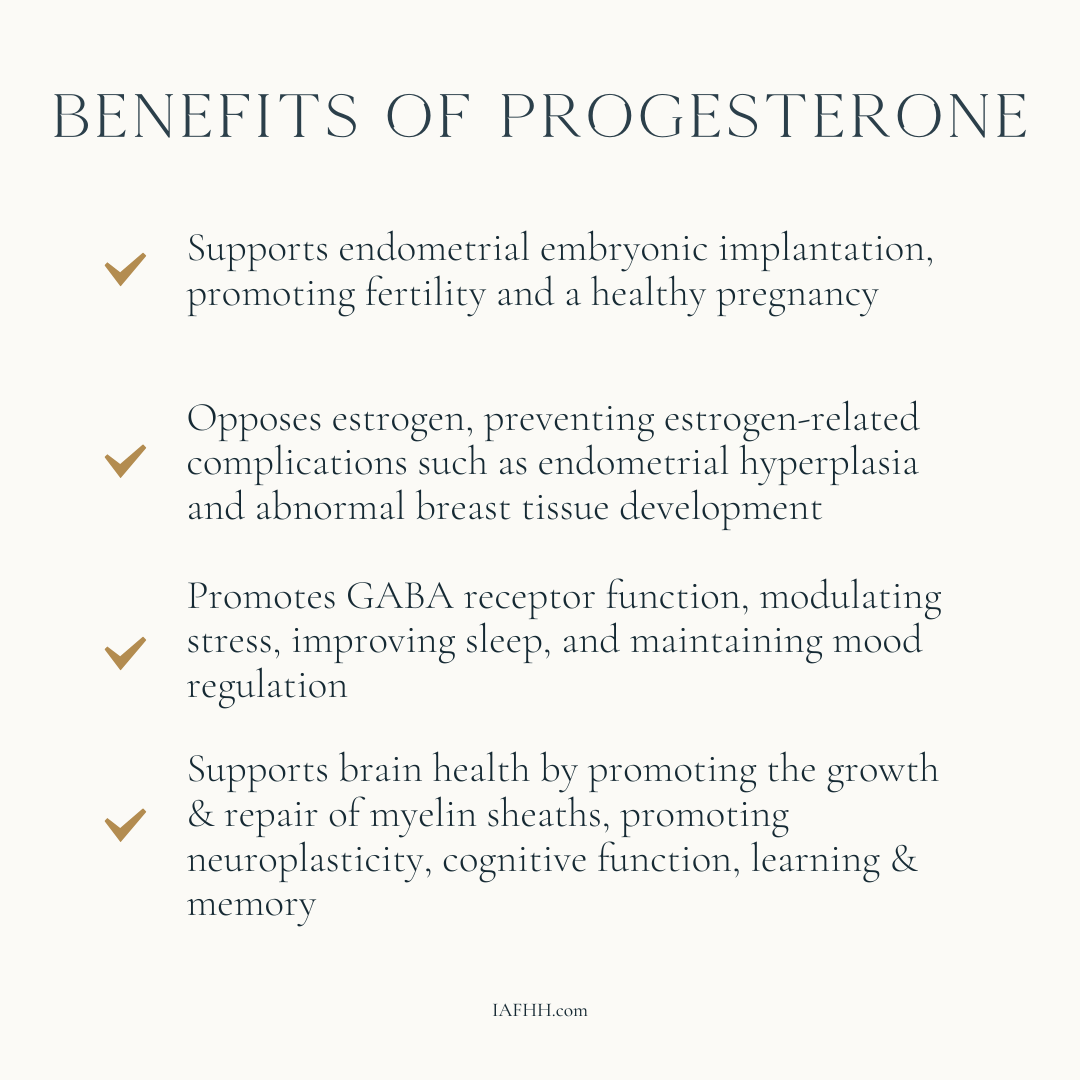
Benefits of Progesterone:
- Progesterone produced from the corpus luteum after ovulation helps to protect the endometrial lining within the uterus by inhibiting excessive estrogen action. (9) Excess estrogen action within the uterus can potentially lead to Endometrial Hyperplasia which can increase one’s risk of developing endometrial cancer. Progesterone also supports breast health by inhibiting excessive estrogen action, which can factor into the onset & proliferation of breast cancer cells. (10)
- The metabolism of progesterone contributes to the increased receptor function of GABA, an inhibitory neurotransmitter that reduces the excitability of neurons in the nervous system, playing an important role in modulating stress, improving sleep, and maintaining mood regulation. (11)
- Progesterone supports brain health by promoting the growth & repair of myelin sheaths. (12) Thus, progesterone can help to promote the brain’s neuroplasticity which can improve cognitive function, learning & memory.
If ovulation doesn’t occur, or ovulation isn’t as robust as it should be, this can lead to diminished, or lowered progesterone production, respectively.
Without enough progesterone, this allows estrogen to dominate during the luteal phase which may contribute to the onset of PMS symptoms, cycle irregularities, heavy periods, menstrual migraines, and breast tenderness as well as difficulty getting & staying pregnant.

The Negative Impact of Hormonal Birth Control
Although we’ve just discussed a handful of benefits to hormone health outside of fertility, some women, and even health practitioners, are still under the impression that ovulation and menstruation have no impact beyond reproductive function.
This leads many to opt for hormonal birth control as a way to not only prevent pregnancy but also to “regulate” hormone imbalances.
How Hormonal Birth Control Works
Although it may appear that hormonal birth control is regulating hormones and one’s menstrual cycle, it is actually doing quite the opposite.
The synthetic hormones (progestin & ethinylestradiol) found within hormonal contraceptives work to inhibit ovulation by interfering with the body’s natural hormone production and balance. (13) Unfortunately, these synthetic hormones are not the same as natural estrogen & progesterone, thus, they cannot and do not have the same beneficial effects as mentioned in this article. Rather, these synthetic hormones wind up suppressing natural hormone production, rather than regulating them.
This misunderstanding of how hormonal contraceptives work is a huge disservice to women in the world and contributes to the vast majority of health-related problems that women face both during and after the discontinuation of hormonal birth control.
Just as hormone balance is important for many areas outside of reproductive function — such as brain health, sleep regulation, bone density, heart health, breast health, and more — hormonal contraceptives may negatively impact these areas of health.

Why Fertility Matters Even If You Aren’t a “Fertility Specialist”
As we’ve discussed extensively throughout this article, just about everything in regard to ovulation, hormones, and fertility matters for many reasons outside of reproduction.
This is why, even if you don’t position yourself as a “fertility specialist”, considering your female client’s fertility, ovulatory status, and hormone balance are incredibly important factors in providing them the most superb support possible — regardless of your niche.
Fertility and ovulation are completely natural and important biological processes that happen for a reason. The many benefits of ovulation beyond conception that have been listed in this article are only the tip of the ice burg when it comes to why fertility matters.
As a women’s health practitioner, it’s your responsibility to inform yourself of the benefits of these hormones, why fertility matters outside of reproductive health, and how hormones and fertility can impact all areas of your female client’s health and well-being.
After all, women’s health is so much more than female fecundity, and that deserves to be recognized and supported just as much as those who are fertility-focused.
Looking for More Resources?
Want more tools and strategies for supporting your client’s fertility and ovulatory health so you can maximize your ability to support them in all areas of their life? Be sure to check out our practitioner training, the IAFHH Functional Hormone Specialist Certification Program.
By receiving the cutting-edge research and specialized education available in our program, you will quickly excel in your private practice and become the go-to hormone health expert in your community. In this program, we support you with all the tools, resources & information you need to expand your expertise in functional hormone health, get your female clients to achieve real & lasting results, and excel in your women’s health practice.

About the Author
Ashe Milkovic, NTP, IC-FHS, FBCS
Ashe is the founder and CEO of The International Association for Functional Hormone Health. She has a passion for spreading awareness about the power of functional nutrition for optimizing hormones & fertility, and her mission is to build community and safe space for other practitioners and aspiring learners to expand their knowledge and expertise in functional hormone health.
Article Sources
- T. Wasilewski, M. Łukaszewicz-Zając, J. Wasilewska, B. Mroczko, Biochemistry of infertility, Clinica Chimica Acta, Volume 508, 2020, Pages 185-190, ISSN 0009-8981, https://doi.org/10.1016/j.cca.2020.05.039
- Young, S. L. (2013). Oestrogen and progesterone action on endometrium: A translational approach to understanding endometrial receptivity. Reproductive BioMedicine Online, 27(5), 497–505. https://doi.org/10.1016/j.rbmo.2013.06.010
- Borahay MA, Asoglu MR, Mas A, Adam S, Kilic GS, Al-Hendy A. Estrogen Receptors and Signaling in Fibroids: Role in Pathobiology and Therapeutic Implications. Reprod Sci. 2017 Sep;24(9):1235-1244. doi: 10.1177/1933719116678686. Epub 2016 Nov 20. PMID: 27872195; PMCID: PMC6344829.
- McGlade, E.A.; Miyamoto, A.; Winuthayanon, W. Progesterone and Inflammatory Response in the Oviduct during Physiological and Pathological Conditions. Cells 2022, 11,1075.
- Shepherd JE. Effects of estrogen on congnition mood, and degenerative brain diseases. J Am Pharm Assoc (Wash). 2001 Mar-Apr;41(2):221-8. doi: 10.1016/s1086-5802(16)31233-5. PMID: 11297335.
- Hui Yan, Wangbao Yang, Fenghua Zhou, Xiaopeng Li, Quan Pan, Zheng Shen, Guichun Han, Annie Newell-Fugate. Yanan Tian, Ravikumar Majeti, Wenshe Liu, Yong Xu, Chaodong Wu, Kimberly Allred, Clinton Allred, Yuxiang Sun, Shaodong Guo. Estrogen Improves Insulin Sensitivity and Suppresses Gluconeogenesis via the Transcription Factor Foxo1. Diabetes 1 February 2019; 68 (2): 291–304. https://doi.org/10.2337/db18-0638
- Väänänen HK, Härkönen PL. Estrogen and bone metabolism. Maturitas. 1996 May;23 Suppl:S65-9. doi: 10.1016/0378-5122(96)01015-8. PMID: 8865143.
- Riggs BL. The mechanisms of estrogen regulation of bone resorption. J Clin Invest. 2000 Nov;106(10):1203-4. doi: 10.1172/JCI11468. PMID: 11086020; PMCID: PMC381441.
- Kim JJ, Chapman-Davis E. Role of progesterone in endometrial cancer. Semin Reprod Med. 2010 Jan;28(1):81-90. doi: 10.1055/s-0029-1242998. Epub 2010 Jan 26. PMID: 20104432; PMCID: PMC4767501.
- Chang KJ, Lee TT, Linares-Cruz G, Fournier S, de Ligniéres B. Influences of percutaneous administration of estradiol and progesterone on human breast epithelial cell cycle in vivo. Fertil Steril. 1995 Apr;63(4):785-91. PMID: 7890063.
- Follesa P, Serra M, Cagetti E, Pisu MG, Porta S, Floris S, Massa F, Sanna E, Biggio G. Allopregnanolone synthesis in cerebellar granule cells: roles in regulation of GABA(A) receptor expression and function during progesterone treatment and withdrawal. Mol Pharmacol. 2000 Jun;57(6):1262-70. PMID: 10825399.
- Schumacher M, Hussain R, Gago N, Oudinet JP, Mattern C, Ghoumari AM. Progesterone synthesis in the nervous system: implications for myelination and myelin repair. Front Neurosci. 2012 Feb 8;6:10. doi: 10.3389/fnins.2012.00010. PMID: 22347156; PMCID: PMC3274763.
- J. Spona, W. Feichtinger, Ch. Kindermann, C. Wünsch, K. Brill, Inhibition of ovulation by an oral contraceptive containing 100 μg levonorgestrel in combination with 20 μg ethinylestradiol. Contraception, Volume 54, Issue 5, 1996, Pages 299-304, ISSN 0010-7824, https://doi.org/10.1016/S0010-7824(96)00183-7
