Gut dysfunction is often associated with uncomfortable gastrointestinal symptoms including indigestion, heartburn, food sensitivities, bloating, and constipation. But did you know that digestive dysfunction can also manifest within the body in other less obvious ways through its impact on hormones and reproductive organs?
This occurs because the gastrointestinal system does not operate in isolation. The gastrointestinal organs not only sit in very close physical proximity to reproductive organs, but they are also physiologically linked to nearly every other internal organ system and enzymatic pathway, including the endocrine and reproductive organs.
When you consider the biochemistry and metabolic pathways that operate within organ systems it becomes clear just how interconnected these systems are. In fact, the gut has everything to do with hormone balance and vice versa.
Hormones & The Gut – Two Peas In A Pod
It is no surprise then, that functional issues originating within the gut can wreak havoc on areas of your client’s health & well-being, such as their hormone balance. In turn, hormone imbalances can also interfere with gut health in important ways.
These inter-relationships can make supporting a client’s gut dysfunction way more complex than simply recommending a probiotic supplement. However, understanding these connections also gives the practitioner the ability to support a client who is seeking to make long-lasting positive changes to both their gut and hormonal health.
When looking at a client’s health from a functional health perspective, we have the opportunity to take a step back and evaluate the bigger picture of what’s actually going on. This article will walk you through the intimate connections between hormone imbalance and gut health so you can better support your female clients in all areas of their health & well-being — from digestion to reproduction.

Recognizing Symptoms of Hormone Imbalance
It is commonly assumed that hormone imbalances will present themselves as PMS, painful periods, cycle irregularities, ovulatory failure, and/or infertility. However, they can also show up in other forms that affect our skin, mood, digestion, and more.
Symptoms of a hormone imbalance include:
- Pelvic Pain/Cramping
- Heavy Periods/Clots
- Cycle Irregularities
- Amenorrhea (lack of menses)
- Mood Swings
- Depression/Anxiety
- Vaginal Dryness
- Low Libido
- Breast Tenderness
- Insomnia
- Chronic Fatigue/Brain Fog
- Headaches/Migraines
- Acne/Oily Skin
- Hair Thinning/Breaking
- Bloating/Indigestion
- Constipation/Diarrhea
- Increased or Suppressed Appetite
- Undesired Weight Gain or Loss
- Fertility Struggles or Infertility
Unfortunately, many women are misinformed that such symptoms are a “normal” discomfort associated with their menstrual cycle or are due to conditions unrelated to their hormones. As a result, symptoms of hormonal imbalance frequently go unnoticed or may be confused for other conditions, resulting in conflicting information and advice.

Birth Control & Hormone Health
First, it should be made clear that birth control is not the only option to treat hormonal imbalances. However, women within the United States are frequently prescribed birth control to “manage” their period and hormone symptoms. [1]
A review from 2011 in the United States looked at the use of oral contraceptive pills (OCP) by an estimated 11.2 million women aged 15-44. Their findings indicate that a majority of OCP users (58%) took the pill at least in part for reasons other than contraception, including cramps and menstrual pain (31%); menstrual regulation (28%), acne (14%), endometriosis (4%), and other reasons (11%). [2]
This review also found that 14% of OCP use was exclusively for non-contraceptive purposes, with one-third of teenage girls using OCPs for non-contraceptive purposes. Even amongst women who had never had sex, it was found that at least 762,000 women relied on OCPs solely for non-contraceptive benefits including menstrual pain (57%), menstrual regulation (43%), and acne (26%). [2]
Consider a woman who is experiencing symptoms of a hormone imbalance such as premenstrual mood swings, pelvic cramping, and irregular cycles. From an allopathic health perspective, her first recommendation would likely be over-the-counter pain medications or even the birth control pill to manage her symptoms.
While these options may temporarily help mitigate symptoms, they often don’t address why these symptoms are present in the first place. This is because oral contraceptives typically do not “fix” the conditions they are prescribed to treat such as menstrual pain, cycle dysregulation, endometriosis, or acne. For women who rely on OCPs, these medications may fail to fully mitigate their symptoms, while also increasing the risk of other side effects and complications.
These medications also introduce new concerns, such as access and safe use of these medications, and whether short-term or long-term side effects or complications may be associated with use. Since these recommendations carry risks, they may not be desirable or appropriate for all women, so it is essential that practitioners identify and explain alternatives that exist.
Regardless, in the context of gut dysfunction that stems from a hormone imbalance, taking hormonal birth control may be counterproductive or produce noticeable unwanted side effects. In fact, when gut dysfunction stems from hormonal imbalance, or vice versa, taking hormonal birth control usage may appear to make things worse.

How Hormones Influence the Gut
Hormones and the gastrointestinal system are very closely tied together. For example, you may notice that your clients report suffering from constipation right after ovulation or experiencing looser bowels right before or during their period. Does digestive distress have something to do with female hormonal fluctuations? The answer is yes, of course!
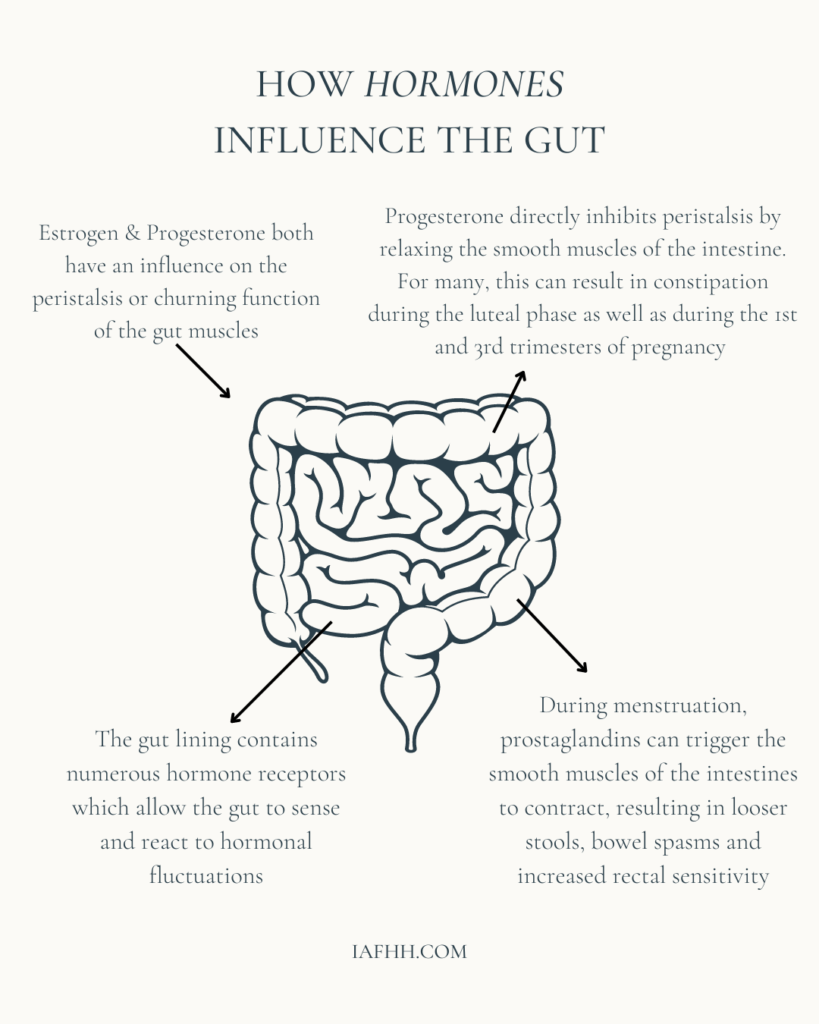
One reason for the connection between hormonal fluctuation and gut function is that the gut lining contains numerous hormone receptors which allow the gut to sense and react to hormonal cues. Some of these receptors directly alter gut motility at various stages throughout the digestive tract. As a result, hormonal changes can influence how often (and how urgently) someone feels the need to go to the bathroom. [3]
It has also been observed that women are much more likely to be diagnosed with IBS (Irritable Bowel Syndrome) than men and many female IBS sufferers see a noticeable difference in symptoms following menopause, with some studies reporting either a decrease or an increase in the severity of IBS symptoms. [3][4][5]
Female sex hormones estrogen & progesterone have both been shown to influence gastrointestinal transit time, which is the speed at which food moved through the gut. [3]
For example, in the upper gastrointestinal tract including the stomach, estrogen can influence delayed gastric emptying, and also alter gastric sensitivity which can contribute to feelings of fullness, bloating, and indigestion. [6]
Increased progesterone can also relax the lower esophageal sphincter in the upper GI tract, which can result in the occasional heartburn and reflux, as is frequently experienced during pregnancy when progesterone levels are elevated. [7]
During the follicular phase, when estrogen levels are high, prolonged gastric relaxation and altered gastric motor function can be seen. A related observation is that women receiving hormone replacement therapy typically have slower gastric emptying rates. [6]
Further along in the intestines, gut motility is achieved through peristalsis or the churning function performed by intestinal muscles as they push food content through the intestines and eventually out of the body. Both estrogen and progesterone have been shown to exert an influence on the coordinated constriction and relaxation of intestinal muscles.
Progesterone can directly inhibit peristalsis by relaxing the smooth muscles of the intestine. For many, elevated progesterone during the luteal phase can result in the onset of constipation. This is also a common symptom during the first and third trimesters of pregnancy when progesterone is at its highest. [8]
Right before menstruation, sex hormone levels decrease to their lowest point, and prostaglandins, which are hormone-like chemicals, begin to trigger the contraction of the uterus to expel its lining resulting in a period. However, prostaglandins can also trigger the contraction of the smooth muscles of the intestines, resulting in looser stools, bowel spasms, and increased rectal sensitivity. [9]
Of course, there are other causes for gastrointestinal discomfort or bowel irregularities, including nutrition, stress, food intolerances, and infection. However, when attempting to determine the impacts of factors such as stress, or illness, we mustn’t overlook the multiplicity of ways in which hormones influence the overall function of the gastrointestinal system alongside other factors.
As a result, hormone imbalances that disrupt digestion and lead to an increase in digestive symptoms may potentially increase the likelihood of receiving an IBS misdiagnosis. In this case, attempting to treat IBS symptoms without addressing the underlying hormonal condition would be unlikely to yield lasting positive improvements and might make matters worse.
In the context of gut dysfunction that stems from a hormone imbalance, it is important to remember that hormonal birth control does not typically “fix” an underlying hormone imbalance, and taking synthetic hormones may even be counterproductive to gut function and produce unwanted digestive side effects.

How the Gut Influences Hormones
Since hormone imbalances and digestive disturbances can create feedback loops that continue to alter one another, it can leave clients feeling like they are in a catch-22 situation. As their practitioner, should you first focus on supporting their digestion or their hormones? The answer is simple, both.
Hormone imbalances can be difficult to control once established. However, they are entirely possible to correct with the right strategy & approach. A fundamental part of that strategy is to support your client’s gastrointestinal health.
One particular type of hormone imbalance that is closely related to gut function is Estrogen Dominance. This imbalance often results in a cycle that has more severe cycle-related symptoms and exacerbated digestive issues.
Estrogen dominance can stem from either increased levels of estrogen and/or decreased levels of progesterone. However, to understand why estrogen dominance is closely tied to gut function, it is important to understand the role of the gut in estrogen metabolism within the body.
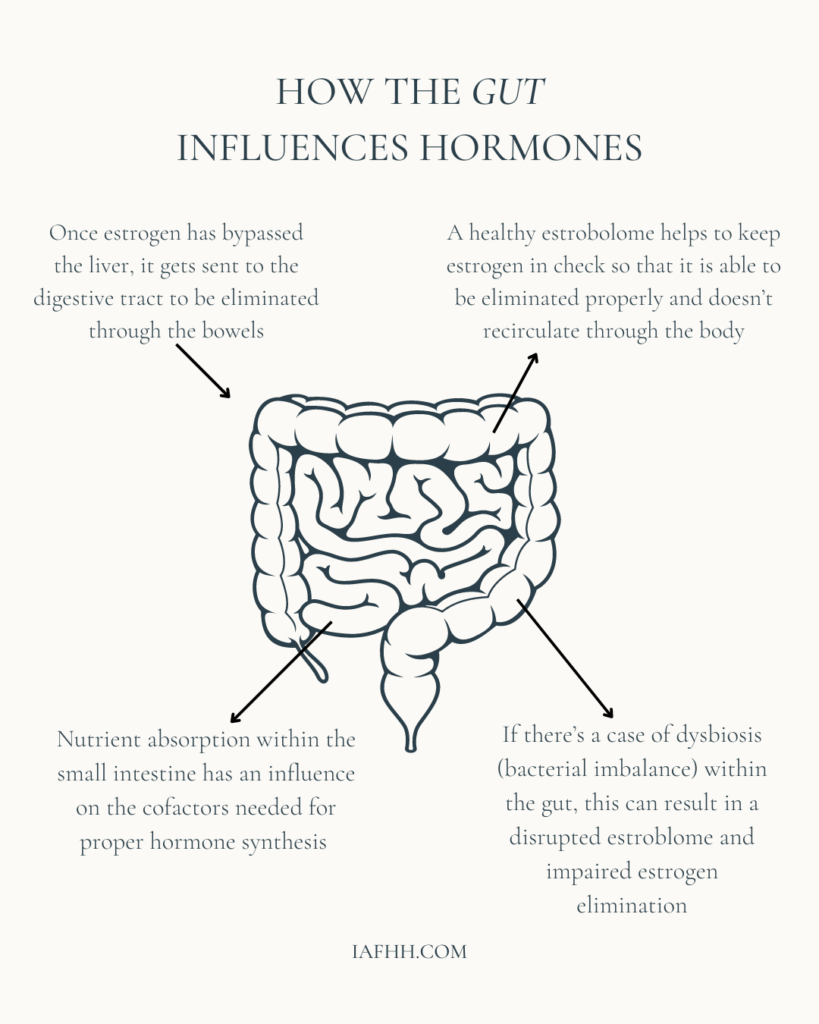
Estrogen, although produced naturally within the body, can be damaging if not detoxified properly. Thus, once excess estrogen has bypassed the liver, it gets sent on to the digestive tract through the bile to be eliminated through the bowels. Specifically, via metabolic breakdown by the many bacteria which reside there. [10]
The total population of gut bacteria and other microorganisms refers to what we call our gut microbiome. An enormous variety of bacterial species exist within the microbiome, including beneficial bacteria, known as symbionts. These organisms help us to break down our food, produce vital nutrients and protect us from foreign pathogenic invasions. [11]
The microbiome is important to hormonal health since individual differences in which bacteria are present can directly influence hormone metabolism, specifically when it comes to the detoxification process of estrogen. [12]
We call the subset of bacteria in the microbiome which provide an estrogen-regulating function the estrobolome. A healthy estrobolome is needed for estrogen to be eliminated properly. This keeps estrogen from being recirculated through the body where it could disrupt both digestive and reproductive organ function. [10]
Not all organisms within the gut microbiome are working in harmony to optimize our health. Both the microbiome and the estrobolome can change in composition and behavior over the course of our lifespan, and both can be dramatically altered by changes in age, diet, illness, and by the use of antibiotics and other medications. [11]
Dysbiosis (bacterial imbalances) within the gut can result in a disrupted estrobolome. In this case, innocuous or non-beneficial bacterial species can overgrow to harmful levels.
Such bacterial overgrowth can include bacteria that contain beta-glucuronidase activity which allows them to interfere with the estrogen that’s being eliminated through deconjugation. This allows estrogen to be reabsorbed by the body and return into circulation. This can lead to worsening cases of estrogen dominance and increased levels of toxicity. [13]
The internal stress of dysbiosis or pathogenic overgrowth by yeasts or parasites can also cause an increase in inflammation. This can trigger more prostaglandins, resulting in more painful periods, as well as an increase in the stress hormone, cortisol. [14]
A rise in cortisol due to stress can even directly lower progesterone levels, resulting in further hormonal and reproductive complications, and furthering the imbalance of estrogen and progesterone. [15]
Later in life, women experiencing menopause may see a drop in estrogen production co-occurring with changes in the estrobolome that together can precipitate a sharp reduction in circulating estrogen. [16]
Either an excess or absence of estrogen can affect outcomes related to cognition, sleep, fertility, and estrogen-modulated diseases, such as obesity, cancer, cardiovascular disease as well as endometrial hyperplasia, endometriosis, polycystic ovarian syndrome, and more. As a result, gut dysfunction can readily contribute to symptoms such as low energy, mental fatigue, mood swings, poor cognition & memory, disturbed sleep, and circadian rhythm, in addition to various cycle and fertility-related complications. [16][17][18][19]
Thus, it is important to remember that hormone imbalances are often linked to poor gut function and an imbalanced microbiome. This knowledge helps to explain why supporting gut function and health is often fundamental to correcting a hormonal imbalance – if something goes wrong with either system, it can create a whole host of problems and can spell trouble for the other.

How to Restore Gut Health & Hormone Balance
Hormone imbalances can be difficult to control once established. However, they are entirely possible to correct with the right strategy & approach. Not surprisingly, a fundamental part of that strategy is to support your client’s gastrointestinal health.
When it comes to restoring gut health & function, I often recommend the 5-R Approach to Gut Restoration. Please note that the following protocol is provided for educational purposes only. Please seek appropriate training or counsel before administering supplements or dietary therapies to your clients. If you would like to receive 1:1 mentorship in creating and delivering such protocols to your clients, please view our IAFHH mentorship page here.
The 5-R Approach to Gut Restoration:
- Remove triggers
The process first starts with your client identifying what the main triggers are to their digestive disturbances. This could include, identifying & removing specific food intolerances, and avoiding pro-inflammatory and damaging food substances (processed foods, sugar, gluten, etc.). It may also include a bit of detective work to determine if there’s a case of dysbiosis, yeast overgrowth, or pathogenic invasion that you’d need to correct. If you are not familiar with these steps, you can recommend that your client works with a functional health practitioner to carry out an elimination diet and/or a GI map test and MRT food sensitivity test. - Replace
Once the main triggers are removed from your client’s diet and/or they’ve identified any underlying pathogenic invasions that you’d need to eradicate, the next step is to replace these triggers with well-tolerated foods and supplements. This step in the process provides the basic fundamental building blocks that support your client’s overall GI tract health & function. This may include introducing stomach acid-stimulating supplements, digestive enzymes, fiber, as well as essential vitamins & minerals through a nutrient-dense diet and/or supplementation. Once again, if you are not familiar with these steps, a functional health practitioner will be an excellent resource. - Reinoculate
Sometimes a practitioner will recommend various herbs/supplements to eradicate a pathogenic invasion. Typically, at this point, introducing a high-quality probiotic supplement alongside probiotic-rich foods can help to reinoculate the intestines with beneficial bacteria. The strain, quantity, and source of probiotics are important factors and may be best determined by a functional health practitioner. - Repair
In cases of gut dysfunction, the intestinal lining is often damaged. Inflammation, food intolerances, and dysbiosis can all contribute to the degradation of the intestinal lining. At this step in the process, it is good to bring in supportive & soothing substances that can help to heal & seal the gut lining. Such as Bone Broth, L-Glutamine, MSM, Vitamin C, Vitamin A, Vitamin D, Zinc, etc. - Rebalance
The last step in the process is to incorporate and stick with a supportive dietary & lifestyle plan that helps to keep everything in balance. This might include eliminating or decreasing exposure to certain stressors, supporting digestive function through a maintenance plan, sticking with a highly nutrient-dense and supportive diet, optimizing sleep, and prioritizing stress management.
In Conclusion
Gut health and hormones are intimately connected in even more ways than we may realize. Each system has an influence on and impacts the health outcome of the other. When it comes to promoting hormone balance, supporting gut function is an essential step in the process. At the same time, hormone health is also necessary for proper gut function. So in many ways, we cannot support the optimization of one system without also recognizing and supporting the other.
In addition to gut health, there are many ways to support hormonal health and harmony such as balancing blood sugar, supporting the detoxification pathways, improving ovulatory function, improving nutrient status, and managing stress appropriately.
When making considerations in each of these areas, we inevitably return to the underlying goal of optimizing digestive health and hormonal balance. By understanding the intricate and ancient cyclical dance that connects these two systems, it becomes possible to identify important patterns in your client’s health and find a sure-footed path toward long-lasting, positive change.
Looking for More Resources?
Want more tools and strategies for supporting your client’s hormone health so you can maximize your ability to support them in all areas of their life? Be sure to check out our practitioner training, the IAFHH Functional Hormone Specialist Certification Program.
By receiving the cutting-edge research and specialized education available in our program, you will quickly excel in your private practice and become the go-to hormone health expert in your community. In this program, we support you with all the tools, resources & information you need to expand your expertise in functional hormone health, get your female clients to achieve real & lasting results, and excel in your women’s health practice.

About the Author
Ashe Milkovic, NTP, IC-FHS, FBCS
Ashe is the founder and CEO of The International Association for Functional Hormone Health. She has a passion for spreading awareness about the power of functional nutrition for optimizing hormones & fertility, and her mission is to build community and safe space for other practitioners and aspiring learners to expand their knowledge and expertise in functional hormone health.
Article reviewed, edited, & revised by Liz Cody, IAFHH Research Analyst & Curriculum Advisor
Article Sources
- Reproductive Health Access Project. (2015, March 16). Contraceptive pearl: The non-contraceptive benefits of hormonal contraceptives. Reproductive Health Access Project. Retrieved January 4, 2023, from https://www.reproductiveaccess.org/resource/contraceptive-pearls-not-just-birth-control-non-contraceptive-benefits-hormonal-contraceptives/
- Beyond birth control – guttmacher institute. (n.d.). Retrieved January 4, 2023, from https://www.guttmacher.org/sites/default/files/pdfs/pubs/Beyond-Birth-Control.pdf
- https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/IBS-and-Hormones.pdf
- Lenhart A, Naliboff B, Shih W, Gupta A, Tillisch K, Liu C, Mayer EA, Chang L. Postmenopausal women with irritable bowel syndrome (IBS) have more severe symptoms than premenopausal women with IBS. Neurogastroenterol Motil. 2020 Oct;32(10):e13913. doi: 10.1111/nmo.13913. Epub 2020 May 29. PMID: 32469130; PMCID: PMC7529855.
- Yang PL, Heitkemper MM, Kamp KJ. Irritable bowel syndrome in midlife women: a narrative review. Womens Midlife Health. 2021 May 31;7(1):4. doi: 10.1186/s40695-021-00064-5. PMID: 34059117; PMCID: PMC8166071.
- Jiang Y, Greenwood-Van Meerveld B, Johnson AC, Travagli RA. Role of estrogen and stress on the brain-gut axis. Am J Physiol Gastrointest Liver Physiol. 2019 Aug 1;317(2):G203-G209. doi: 10.1152/ajpgi.00144.2019. Epub 2019 Jun 26. PMID: 31241977; PMCID: PMC6734369.
- Pregnancy and heartburn: Causes & management. Cleveland Clinic. (n.d.). Retrieved January 4, 2023, from https://my.clevelandclinic.org/health/diseases/12011-heartburn-during-pregnancy
- Alqudah M, Al-Shboul O, Al Dwairi A, Al-U´Datt DG, Alqudah A. Progesterone inhibitory role on gastrointestinal motility. Physiol Res. 2022 Apr 30;71(2):193-198. doi: 10.33549/physiolres.934824. Epub 2022 Mar 28. PMID: 35344673; PMCID: PMC9150547.
- Bernstein MT, Graff LA, Avery L, Palatnick C, Parnerowski K, Targownik LE. Gastrointestinal symptoms before and during menses in healthy women. BMC Womens Health. 2014 Jan 22;14:14. doi: 10.1186/1472-6874-14-14. PMID: 24450290; PMCID: PMC3901893.
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas. 2017 Sep;103:45-53. doi: 10.1016/j.maturitas.2017.06.025. Epub 2017 Jun 23. PMID: 28778332.
- Bull MJ, Plummer NT. Part 1: The Human Gut Microbiome in Health and Disease. Integr Med (Encinitas). 2014 Dec;13(6):17-22. PMID: 26770121; PMCID: PMC4566439.
- Qi X, Yun C, Pang Y, Qiao J. The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes. 2021 Jan-Dec;13(1):1-21. doi: 10.1080/19490976.2021.1894070. PMID: 33722164; PMCID: PMC7971312.
- Ervin SM, Li H, Lim L, Roberts LR, Liang X, Mani S, Redinbo MR. Gut microbial β-glucuronidases reactivate estrogens as components of the estrobolome that reactivate estrogens. J Biol Chem. 2019 Dec 6;294(49):18586-18599. doi: 10.1074/jbc.RA119.010950. Epub 2019 Oct 21. PMID: 31636122; PMCID: PMC6901331.
- de Oliveira GLV, Cardoso CRB, Taneja V, Fasano A. Editorial: Intestinal Dysbiosis in Inflammatory Diseases. Front Immunol. 2021 Jul 30;12:727485. doi: 10.3389/fimmu.2021.727485. PMID: 34394133; PMCID: PMC8362080.
- Herrera AY, Nielsen SE, Mather M. Stress-induced increases in progesterone and cortisol in naturally cycling women. Neurobiol Stress. 2016 Feb 11;3:96-104. doi: 10.1016/j.ynstr.2016.02.006. PMID: 27981182; PMCID: PMC5146195.
- https://journals.asm.org/doi/10.1128/msystems.00273-22
- Salliss ME, Farland LV, Mahnert ND, Herbst-Kralovetz MM. The role of gut and genital microbiota and the estrobolome in endometriosis, infertility and chronic pelvic pain. Hum Reprod Update. 2021 Dec 21;28(1):92-131. doi: 10.1093/humupd/dmab035. PMID: 34718567.
- Wang Z, Wang Z, Lu T, Chen W, Yan W, Yuan K, Shi L, Liu X, Zhou X, Shi J, Vitiello MV, Han Y, Lu L. The microbiota-gut-brain axis in sleep disorders. Sleep Med Rev. 2022 Oct;65:101691. doi: 10.1016/j.smrv.2022.101691. Epub 2022 Aug 31. PMID: 36099873.
- Matenchuk BA, Mandhane PJ, Kozyrskyj AL. Sleep, circadian rhythm, and gut microbiota. Sleep Med Rev. 2020 Oct;53:101340. doi: 10.1016/j.smrv.2020.101340. Epub 2020 May 13. PMID: 32668369.
