Many women and practitioners alike are interested in learning effective ways to support the transition off of birth control.
Although stopping hormonal contraceptives may be as simple as not taking another pill in the pack, or, making an appointment to remove the IUD, the physical transition off birth control can be a bit more nuanced, often resulting in uncomfortable symptoms such as acne, migraines, facial hair growth, weight gain, and/or frustrating struggles with fertility.
To avoid these undesired symptoms, supporting your clients physically through the transition is an important consideration to have as their healthcare practitioner.
This article will share with you why certain symptoms present when discontinuing the pill, and how you can support your clients to have a more smooth and seamless transition off of birth control.

Why Hormonal Birth Control is so Popular
Hormonal birth control (HBC) is a commonly used & prescribed medication that introduces the synthetic hormones, Ethinylestradiol and/or Progestin, shutting off a woman’s natural hormonal fluctuations and preventing pregnancy up to 99% of the time.
As a whole, HBC is favored not only due to its effectiveness in preventing pregnancies but also for its ability to relieve hormonal-based symptoms such as period cramps, PMS, cycle irregularities, and hormonal acne.
This has led HBC to be prescribed for numerous women’s health issues, including as a treatment plan for more serious conditions such as PCOS, endometriosis, fibroids, and ovarian cysts.
What the statistics show
In the United States, on average, 99% of sexually active women have used at least one contraceptive method at some point in their life, and in 2020, the KFF Women’s Health Survey reported that nearly 65% of women in their reproductive stages currently use birth control. (1) (2)
However, the usage of birth control for managing cycle symptoms averages nearly 58% of overall users, meaning that only about 42% use birth control for preventing pregnancy alone. (3)
This means that over half of birth control users are using it for reasons other than contraceptive purposes.
These numbers have accumulated over time and are continuing to rise as HBC usage becomes more widely accepted as normal preventative care within the healthcare system.
The History of Birth Control Usage
Contraceptive methods have been known to be used since 3000 BCE, however, the first oral pill contraceptive, Enovid, wasn’t invented until 1960. (4)
Enovid was created through a mixture of synthetic hormones similar to natural progesterone and estrogen. It was found that the introduction of these compounds suppressed natural hormone production resulting in temporary infertility.
The invention of Enovid ultimately sparked feminist conversation all around the world as it finally gave women the opportunity to be free and in control of their reproductive choices, making a huge step in the evolution of feminism.
Although the history of how the pill came to fruition is based upon a past of feminism and bodily autonomy, over time its usage has only led to further oppression of women’s reproductive health and rights.
Is Birth Control Still Advantageous?
With the knowledge we have today about women’s reproductive health, as well as the technology that’s available to us, solely referring to HBC as the only effective option for pregnancy prevention and symptom management is a great disservice to women.
The problem lies not just within the product itself, nor its ability to provide women with reproductive freedom, but rather, the problem lies with the reproductive healthcare system incessantly promoting its usage whilst not disclosing the true function of the pill and the disruptive effects that it has on women’s reproductive health, not to mention the added risks and side effects that can accompany it.

How Hormonal Birth Control Works
The combination of ethinylestradiol and progestin found within hormonal birth control (most commonly the combined contraceptives such as the pill, patch, and Nuvaring) work together to inhibit the body’s natural hormonal fluctuations, preventing pregnancy through three primary mechanisms.
- Stopping the cyclical fluctuation of natural hormones such as FSH, LH, Estrogen, and Testosterone, which inhibits the process of ovulation
- Creating a thick mucus plug within the cervix making it difficult for sperm to swim up into the uterus & fallopian tubes to fertilize an egg
- Thinning the uterine lining making the uterine environment unfavorable for implantation of a fertilized egg (this part is also what contributes to a lighter, more ‘manageable’ period when on the pill)
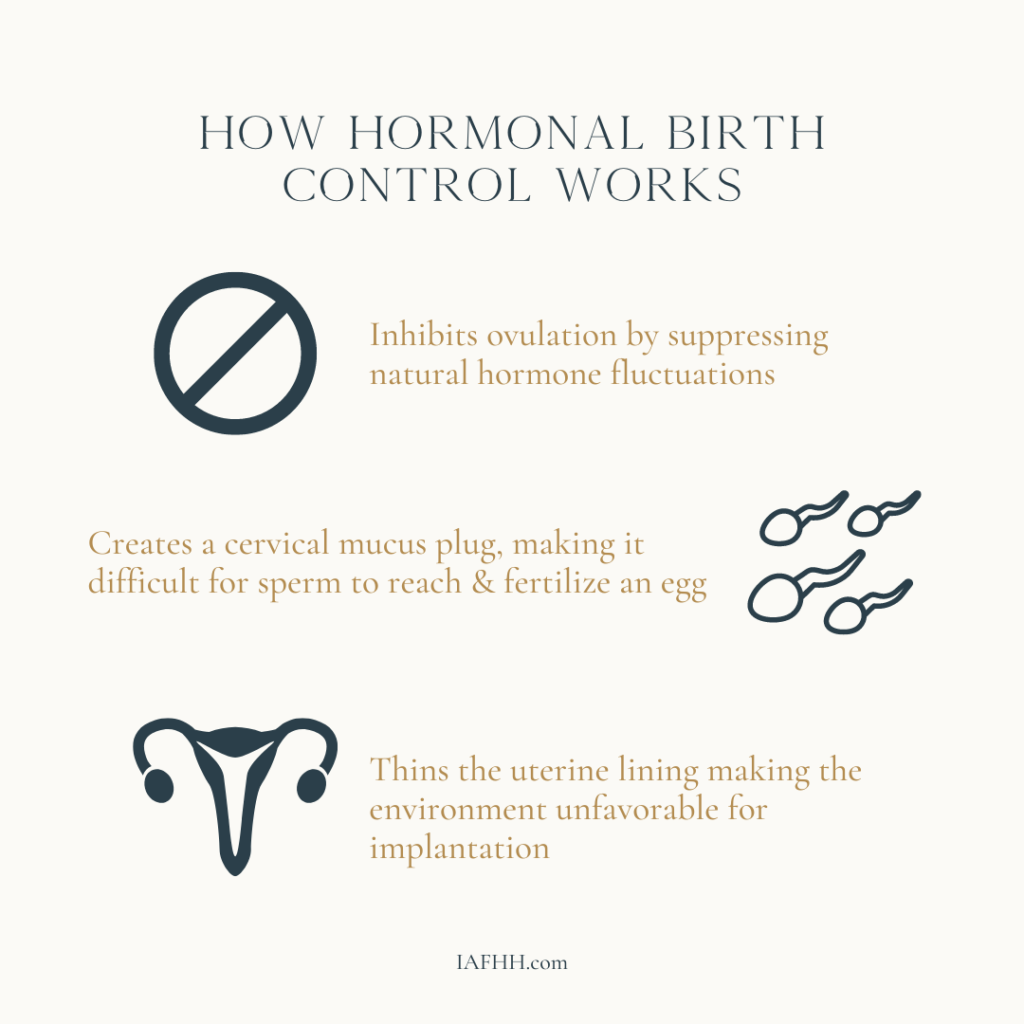
Although these actions may seem harmless, they can have more of an impact on the body than you may expect.
For example, HBC can cause deficiencies in certain nutrients such as B vitamins, Vitamin C, Vitamin E, Magnesium, Zinc & Selenium, and may cause an increased risk for blood clotting, heart attack, stroke, and cancer. (5) (6) (7)

Transitioning Off of Birth Control
Many women experience complications and adverse reactions from taking hormonal birth control. Symptoms such as mood swings, depression, nausea, headaches, weight gain, and decreased libido, are just a few that are commonly reported.
However, instead of seeing these symptoms as serious signs that the body is reacting adversely to the synthetic hormones, many physicians lean on offering additional prescriptions to mitigate the symptoms, or they may provide the patient with an alternative type of hormonal birth control in hopes that they won’t cause the same reactions.
Unfortunately, many women prescribed HBC are not disclosed the potential risks and side effects involved, many of which include the common symptoms that are experienced and reported.
Beyond this, when women are ready to come off of the pill (whether that be to achieve pregnancy, to experience menopause, or for other personal reasons), it is not common that they are informed that their symptoms will likely return as the root cause was never actually addressed.
Post-Birth Control Syndrome
For those who take HBC to manage cyclical discomfort, coming off the pill can trigger the return of symptoms (and often with a vengeance).
Due to the suppression HBC has on natural hormones (and imbalances thereof), using HBC as a treatment can potentially make matters worse on the inside by not correcting the underlying issue.
In addition, long-term HBC usage can trigger thyroid issues, impair glucose metabolism, and contribute to an increase in sex hormone-binding globulin (SHBG), which can lead to a host of other complications resulting in even more undesired symptoms post-pill. (8) (9) (10)
Post-Pill Androgen Rebound
Another common issue that can arise after hormonal birth control usage is post-pill androgen rebound. This often results in symptoms similar to PCOS, and may even result in a PCOS misdiagnosis post-pill.
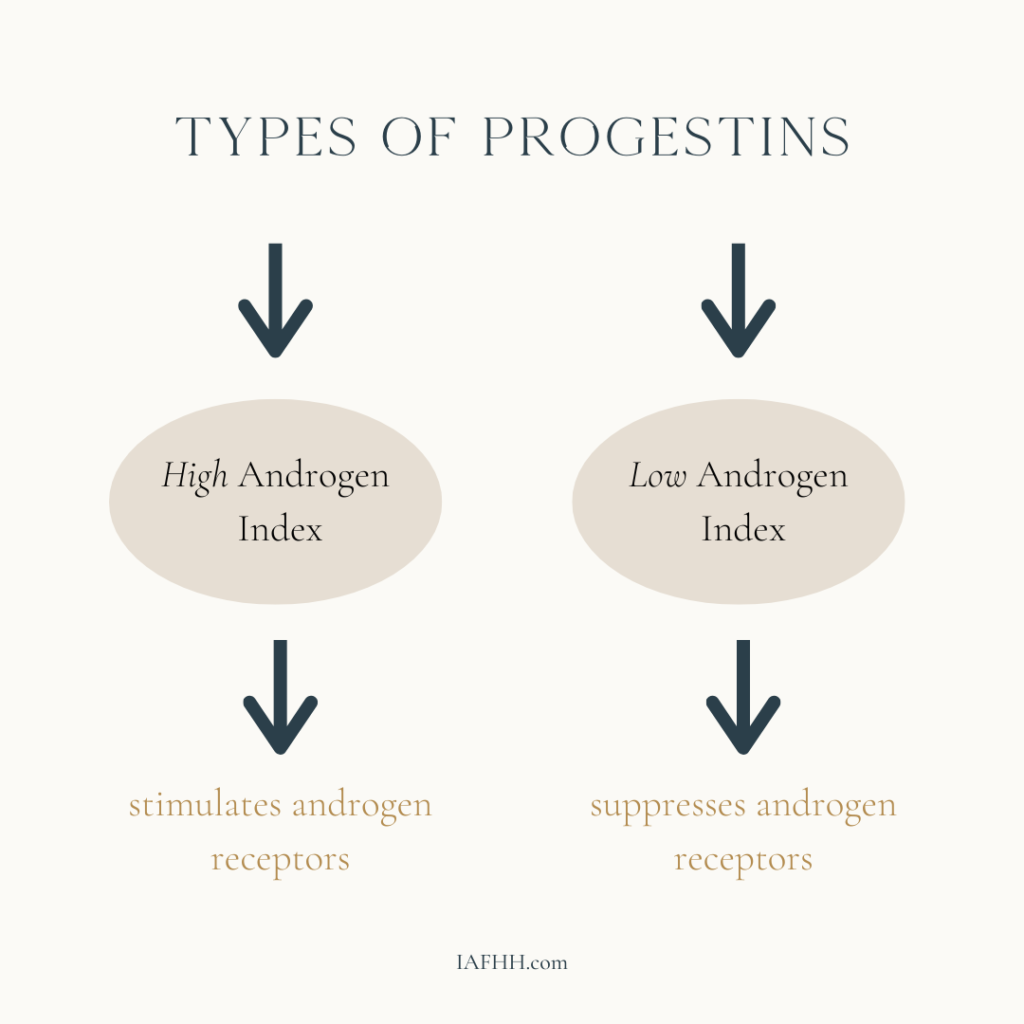
Certain progestins, such as Levonorgestrel, Norgestrel, and Norethindrone, have a “high androgen index” meaning they can stimulate androgen receptors, including DHT. (11)
This is why these forms of progestin contraceptives are usually associated with side effects such as acne and hair loss.
Other forms of progestins, such as Drosperinone, Norgestimate, and Ethynodiol Diacetate (often found in combined contraceptives), have a “low androgen index” meaning they suppress androgen levels. (11)
Although this may seem beneficial, the body typically compensates for the suppression by attempting to stimulate even more androgen production, especially once the contraceptive has been discontinued.
This post-pill androgen rebound effect can result in symptoms such as cystic acne, facial or nipple hair growth, hair thinning, and irregular cycles, mimicking PCOS.
Thankfully, these symptoms are usually temporary, but they can last anywhere between 1- 2 years if not supported.

Supporting The Transition
If your clients have decided to transition off of birth control there are a few things to consider.
For one, expect that it may take time for their hormones to stabilize and ovulation to occur once more. The time that it takes for cycles to regulate can vary from person to person. For some, it may take anywhere from 3-12 months. Therefore, it is advised to recommend your clients come off of HBC roughly 6-12 months before planning to conceive.
To help support the process, here are a few ways you can support their body through the detoxification and re-establishing of proper HPO (hypothalamic-pituitary-ovarian) communication.
High-Quality Multivitamins:
A high-quality multivitamin can help to ensure that any nutritional deficiencies are addressed when your client comes off of the pill. In addition to this, promoting a nutrient-dense diet is highly recommended to make sure they are fully supported nutritionally. This is especially true if they were on hormonal birth control for an extended period of time.
If your client is on any other form of medication, you can double-check for potential nutrient deficiencies by using a drug-nutrient interaction checker available through Mytavin or Integrative Therapeutics.
Digestive & Blood Sugar Support:
Ethinylestradiol and progestin can impact more than just the endocrine system and hormonal balance. These synthetic hormones can also have a negative impact on a person’s digestive function and blood sugar regulation.
For example, HBC can disrupt the microbiome, contributing to an increase of dysbiotic bacteria and beta-glucuronidase activity. In turn, this can impair proper estrogen elimination and interfere with overall digestive function. (12)
The androgenic aspects of specific progestins may also interfere with proper insulin sensitivity, resulting in more challenges post-pill with maintaining blood sugar balance and regulation.
Therefore, supporting these areas strategically both during and post-pill can be incredibly important for helping to promote hormone regulation and ovulatory function.
HPO-support:
A functional hypothalamic-pituitary-ovarian axis is an integral part of maintaining hormone balance and ovulatory health. This axis is important for stimulating communication between the brain and the ovaries which is necessary for hormone production and ovulation.
For many, HBC can disrupt this vital communication from the brain to the ovaries. When this happens, it may elongate the time it takes for one’s cycle to return post-pill.
The HPO system is very intimately connected with other hypothalamic-pituitary axes, such as the HPA (adrenal) and HPT (thyroid) axes. Therefore, promoting stress resiliency and metabolic health is incredibly important for maintaining healthy HPO axis function.
Glandular therapy, such as with glandular pituitary/hypothalamus (Cytozyme PT-HPT from Biotics Research) and glandular ovary (Cytozyme-O from Biotics Research) may be a great option for supporting individuals with a sluggish HPO-axis.
Disclaimer: Please take precautions recommending specific support supplements & glandular therapy. If you have not been properly trained on administration and monitoring, please seek support. Check out our mentorship services for additional support with fine-tuning your client protocols.

In Conclusion
Hormonal birth control may be effective at preventing pregnancy and mitigating symptoms of hormonal imbalance. However, it can only do so at a great cost to a woman’s overall health and well-being.
With how normalized and accessible HBC has become, we need to be considering ways to provide the public with more thorough education and resources for alternative hormone support strategies and pregnancy prevention.
The Fertility Awareness Method is an incredible resource and option for those desiring non-hormonal pregnancy prevention and family planning.
In addition, our IAFHH Certified Functional Hormone Specialist Practitioner Directory is also a great resource for finding practitioners well-versed in supporting hormone balance naturally.
Want more resources?
Want more tools and strategies for supporting your client’s hormone health so you can maximize your ability to support them in all areas of their life? Be sure to check out our practitioner training, the IAFHH Functional Hormone Specialist Certification Program.
By receiving the cutting-edge research and specialized education available in our program, you will quickly excel in your private practice and become the go-to hormone health expert in your community. In this program, we support you with all the tools, resources & information you need to expand your expertise in functional hormone health, get your female clients to achieve real & lasting results, and excel in your women’s health practice.

About the Author
Ashe Milkovic, NTP, IC-FHS, FBCS
Ashe is the founder and CEO of The International Association for Functional Hormone Health. She has a passion for spreading awareness about the power of functional nutrition for optimizing hormones & fertility, and her mission is to build community and safe space for other practitioners and aspiring learners to expand their knowledge and expertise in functional hormone health.
Article Sources
- Daniels K, Mosher WD and Jones J. Contraceptive methods women have ever used: United States, 1982–2010, National Health Statistics Reports, 2013, No. 62, https://www.cdc.gov/nchs/data/nhsr/nhsr062.pdf
- KFF Women’s Health Survey 2020. https://img.datawrapper.de/Q7Jen/full.png, https://www.kff.org/womens-health-policy/issue-brief/womens-sexual-and-reproductive-health-services-key-findings-from-the-2020-kff-womens-health-survey/
- Beyond brith control: The overlooked benefits of oral contraceptive pills. (n.d.). Retrieved November 2, 2022, from https://www.guttmacher.org/sites/default/files/report_pdf/beyond-birth-control.pdf
- Khan F, Mukhtar S, Dickinson IK, Sriprasad S. The story of the condom. Indian J Urol. 2013 Jan;29(1):12-5. doi: 10.4103/0970-1591.109976. PMID: 23671357; PMCID: PMC3649591.
- Palmery M, Saraceno A, Vaiarelli A, Carlomagno G. Oral contraceptives and changes in nutritional requirements. Eur Rev Med Pharmacol Sci. 2013 Jul;17(13):1804-13. PMID: 23852908.
- Kaminski P, Szpotanska-Sikorska M, Wielgos M. Cardiovascular risk and the use of oral contraceptives. Neuro Endocrinol Lett. 2013;34(7):587-9. PMID: 24464000.
- Oral contraceptives (birth control pills) and cancer risk. National Cancer Institute. (n.d.). Retrieved November 1, 2022, from https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/oral-contraceptives-fact-sheet
- Qiu Y, Hu Y, Xing Z et al. Birth control pills and risk of hypothyroidism: a cross-sectional study of the National Health and Nutrition Examination Survey. 2007–2012 BMJ Open 2021;11:e046607. doi: 10.1136/bmjopen-2020-046607
- Cortés ME, Alfaro AA. The effects of hormonal contraceptives on glycemic regulation. Linacre Q. 2014 Aug;81(3):209-18. doi: 10.1179/2050854914Y.0000000023. PMID: 25249703; PMCID: PMC4135453.
- Panzer C, Wise S, Fantini G, Kang D, Munarriz R, Guay A, Goldstein I. Impact of oral contraceptives on sex hormone-binding globulin and androgen levels: a retrospective study in women with sexual dysfunction. J Sex Med. 2006 Jan;3(1):104-13. doi: 10.1111/j.1743-6109.2005.00198.x. PMID: 16409223.
- Moses, S. (2022, October 29). Progestin androgenic activity. Family Practice Notebook. Retrieved November 1, 2022, from https://fpnotebook.com/gyn/pharm/PrgstnAndrgncActvty.htm
- Javurek AB, Spollen WG, Johnson SA, Bivens NJ, Bromert KH, Givan SA, Rosenfeld CS. Effects of exposure to bisphenol A and ethinyl estradiol on the gut microbiota of parents and their offspring in a rodent model. Gut Microbes. 2016 Nov;7(6):471-485. doi: 10.1080/19490976.2016.1234657. Epub 2016 Sep 13. PMID: 27624382; PMCID: PMC5103659.
