The menstrual cycle is commonly seen as mysterious and unpredictable. Women are called “hormonal” as an insult and their cyclical nature is often viewed as a drawback in today’s modern world. This attitude originates far back in human history, but, fortunately, some of us are challenging the notion today.
As it turns out, the hormonal sequence behind the menstrual cycle is incredibly predictable. In many ways, it influences and is influenced by every other system in the body. In other words, our reproductive health intricately connected to our overall well-being.
As health practitioners, we can use fertility awareness as a tool in our clinical practice to tune into the menstrual cycle. We can then use the information gained to support our client’s hormone health and fertility goals. (i.e. avoiding or achieving pregnancy naturally).
So, what exactly is fertility awareness?
One concept to understand before I discuss this further is that women cannot get pregnant every single day. Pregnancy is only physiologically possible for approximately 6 days out of each cycle, near the time of ovulation. In contrast, men are potentially fertile every day beginning in puberty and throughout most of the rest of their lives.
Fertility awareness is a means of using real-time, observable signs that the female body gives each cycle (biomarkers) to assess hormonal activity and determine whether pregnancy is possible on any given day. Women can learn to identify the infertile and potentially fertile days of their menstrual cycles by incorporating new habits that only take a few minutes per day.
How do these observable fertility signs originate?
Reproductive processes are directed by hormones. Hormones are chemical messengers that travel through the bloodstream to send instructions to the various cells in our bodies.
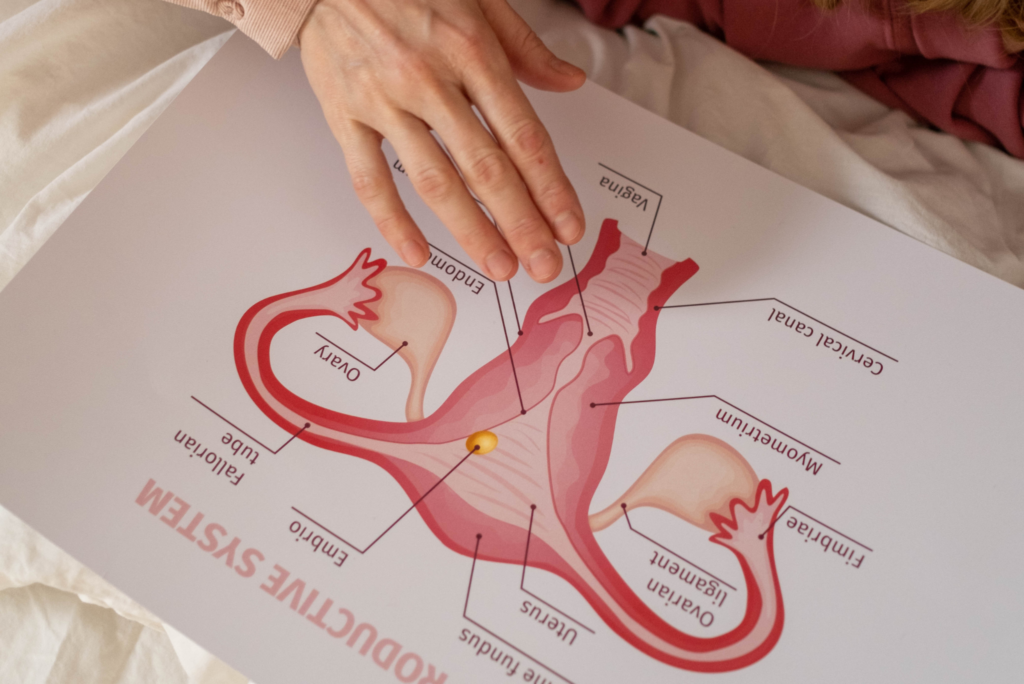
With each cycle, follicle stimulating hormone (FSH) is released from the brain. FSH signals the ovaries to start developing an egg. As that egg matures inside a small sac (follicle) on the ovary, the follicle produces increasing amounts of estrogen.
Estrogen causes changes to occur in the cervix and uterus. The lining in the uterus thickens in preparation for a fertilized egg.
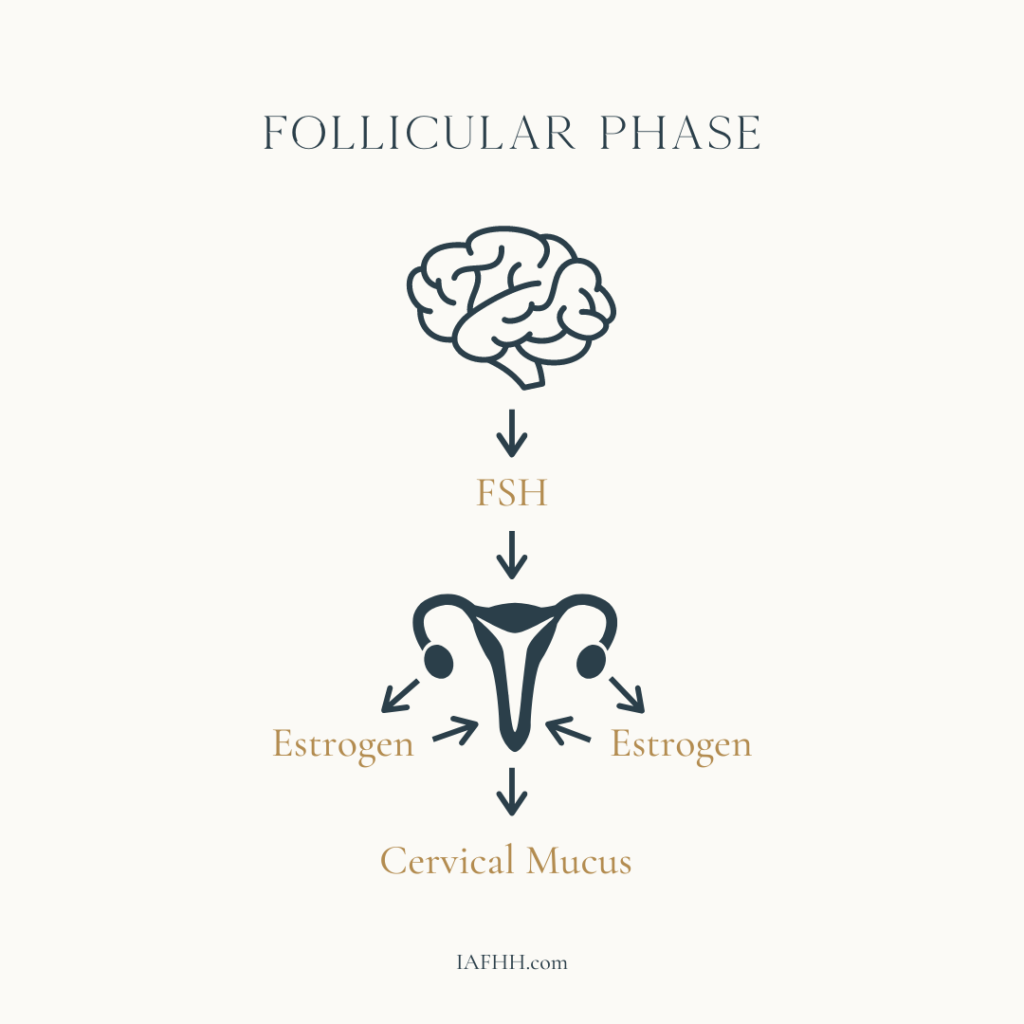
The cervix is full of glands that produce different types of mucus depending on the level and type of hormonal stimulation. As estrogen levels rise, the mucus produced becomes progressively thin, fluid, and slippery. This change can be sensed at the vaginal opening and also observed on toilet paper. This type of cervical mucus keeps sperm cells alive in the cervical crypts for up to 5 days, waiting for ovulation to occur.
When estrogen reaches peak levels, this signals the brain to release luteinizing hormone (LH), which ruptures the follicle in ovulation.
After ovulation, the follicle is transformed into a temporary endocrine gland called the corpus luteum, which secretes the hormone progesterone.
Progesterone causes cervical mucus to abruptly dry up and acts on the uterine lining to further develop it in preparation for a possible pregnancy. It also contributes to thermogenesis, which stimulates a rise in basal body temperature, observable through basal body temperature tracking on a fertility awareness chart.
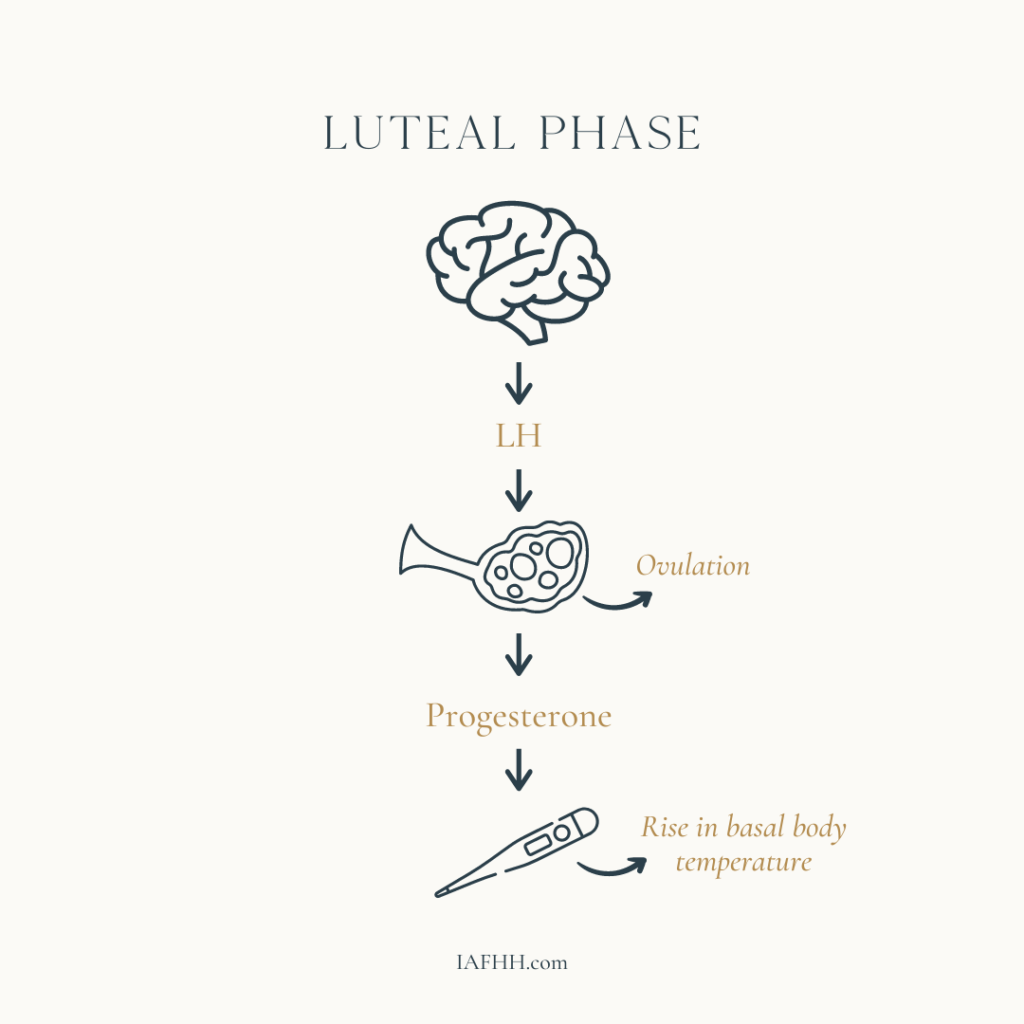
If fertilization does not occur, hormone levels begin to drop off as the corpus luteum disintegrates. This fall in hormones results in the beginning of the next menstruation, marking the start of a new cycle roughly two weeks after ovulation.
Observing the Fertile Window
The key to mastering fertility awareness is learning how to recognize the beginning and end of the ovulatory phase (commonly referred to as the “fertile window”) since this is the only phase in the cycle where pregnancy is possible. Fertility awareness-based methods (FABMs) provide the framework for this.
Fertility Awareness has important benefits aside from simply using the fertility chart to avoid or achieve pregnancy. Tracking observable biomarkers such as bleeding, cervical mucus, LH testing, and basal body temperature (BBT) gives useful information about the state of a woman’s reproductive hormones.
Charting this data allows us to notice if her cycle is following typical patterns for her stage of reproductive life or if she should seek medical attention, or the help of another care provider, to address potential health problems or imbalances.

Different Methods, Different Biomarkers
There are many different FABMs to choose from. These methods are based upon the same science and physiology, but they differ in several important areas: the biomarkers used to determine the different cycle phases, and the guiding philosophy of the people/organizations who originated each method. This NFP (natural family planning) conference is a good overview of some commonly used methods.
In general, we can divide FABMs into broad categories based on the biomarkers used to create the cycle chart:
- Sympto-thermal methods
- Sympto-hormonal methods
- Cervical mucus-only methods
- Temperature-only methods
- Calendar methods
Sympto-thermal methods
Sympto-thermal methods cross-check a woman’s cervical mucus observations and her waking basal body temperatures in order to determine the beginning and end of the ovulatory phase. Examples of sympto-thermal methods include, but are not limited to: Sensiplan, Sympto-Pro, Justisse, FertilityUK, The Well, Serena Canada, NFPTA, and the method taught in Taking Charge of Your Fertility by Toni Weschler (commonly identified in online communities as TCOYF).
Sympto-hormonal methods
Sympto-hormonal methods use urinary hormone measurements, with or without other biomarkers. Marquette Method and Boston Cross Check are both methods that utilize the Clearblue Fertility Monitor to track urinary estrogen and LH metabolites in order to draw the fertile window. They both also have protocols for tracking cervical mucus, BBT, and progesterone test strips.
FEMM is another sympto-hormonal method that utilizes cervical mucus observations and LH strips to determine the cycle phases. There is also a strong emphasis on charting for health, meaning that the charter is encouraged to track any symptoms she may experience throughout her cycle, as well as the approximate volume of her menstruation.
Cervical mucus only methods
Cervical mucus only methods are just what it sounds like – methods that only require the user to track her cervical mucus patterns in order to chart her cycles. These methods include the Billings Ovulation Method, Creighton Method, and Justisse (though there is an optional temperature protocol in Justisse). Billings focuses heavily on sensation felt at the vulva. Meanwhile, Creighton and Justisse focus more on sensation felt by wiping and the very detailed categorization of cervical mucus.
Temperature only methods
Temperature only methods are becoming more common as the use of ovulation/fertility “tracking” apps increases. These apps/devices include Natural Cycles and Daysy. These methods use a proprietary algorithm based on statistical data and the user’s past cycles to estimate the beginning of the ovulatory phase and use BBT to close the fertile window.
The Calendar Method
The Calendar Method (more commonly known as the Rhythm Method) estimates the cycle days that are potentially fertile by calculation – looking at the user’s longest and shortest past cycles to draw the fertile window.
Although this method may be quite reliable for someone who has extremely regular cycles with little variation, for those with irregularities, it does not distinguish between a true menstruation and an anovulatory bleed and does not confirm whether ovulation actually occurred. As a result, this method is less effective than methods that track real-time biomarkers and also doesn’t provide much data about the status of the user’s hormone health.
Pros/Cons of different method types
It’s worth noting that there is no “best” method or one that will be perfect for every potential user. Each FABM has a number of pros and cons. Additionally, each potential user has a different set of lifestyle factors that will influence method choice. These factors include but are not limited to, religious beliefs (or lack thereof), fertility goals (whether they are trying to achieve/avoid pregnancy), cycle type, and reproductive stage.

How Charts Support Hormone Health
Not only is fertility awareness an effective means of avoiding or achieving pregnancy – a woman’s charts can be used as a valuable health record that can be referred to in clinical practice. Imbalances and health concerns can show up as minor changes in hormonal activity, evident long before the onset of disease or more serious symptoms.
Looking at the chart, we can determine if and approximately when she ovulates. Not only that, but we can also observe whether FSH, estrogen, LH, and progesterone appear to be reaching sufficient levels in each cycle – just by looking at her cervical mucus patterns, basal body temperature, and even urinary LH tests.
This is relevant because ovulation is a sign of health. If a woman is in her peak/mid-reproductive years (approx. ages 21-37), it’s expected that she will ovulate about every 24-36 days. If she is not ovulating, this is a sign that the body is under stress and is unable to set reproductive events into motion.
“Ovulation is a sign of health … If she is not ovulating, this is a sign that the body is under stress and is unable to set reproductive events into motion.”
Additionally, in stages of life where ovulation may happen less frequently (puberty, perimenopause), we can still use the chart to ascertain whether there may be areas of health that need to be addressed.
In order to gain the most health information from a fertility chart, women should be encouraged to track symptoms, medications, illness, stress, and lifestyle changes.
Interpreting Hormone Health Biomarkers
Women may find that they experience bothersome symptoms only at certain points in their cycle, indicating a possible hormone imbalance. Charting her patterns cycle after cycle also allows her to observe whether and how stress may impact her biomarkers.
It’s important to remember, however, that hormone imbalances are not a root cause to any symptoms that a woman may experience. Hormones are simply the canaries in the coal mine, so to speak. When there are abnormalities on a cycle chart, this often indicates dysfunction in other body systems.
Blood sugar function, gut health, digestion, stress responses, and thyroid health, for example, are all connected to reproductive hormone function.
Fertility Awareness as a Diagnostic Tool
Another benefit to cycle tracking in clinical practice is that in some cases, it can reduce the number of diagnostic tests needed. Progesterone is a good example to apply here. If a woman has a short luteal phase, 3-4 days of premenstrual spotting, and excessive PMS symptoms, we can infer that she likely has low/insufficient progesterone even without testing.
This also gives us insight into the health of her ovulation in that cycle. A healthy luteal phase requires a healthy follicular phase, so we know that if progesterone is low, there are likely dysfunctions upstream in the hormonal sequence.

Using FABM Charts in Clinical Practice
When our clients make lifestyle changes to better their health, this often becomes evident in the cycle chart within about 2-3 cycles.
Regulating blood sugar and modulating inflammation can result in a healthier ovulatory process and cycle charts that are easier to interpret for fertility management purposes. Stress reduction may help her manage or reduce PMS symptoms. Correcting nutrient deficiencies may help the ovulatory process resume when it has been delayed.
How you can use this knowledge
As a practitioner, educating yourself on the ways in which FAM charts reflect overall health allows you to demonstrate to your clients the effectiveness of the protocols they’re following.
You can use the chart as a progress report of sorts and review the changes together as her health improves. Alternatively, the cycle chart indicates when a protocol may not be serving your client well. For example, if she begins a new supplement, and then ovulation becomes delayed, it will become apparent that this likely isn’t the right protocol for her.
Finally, monitoring health through fertility awareness charting gives women a sense of empowerment and autonomy in managing their health. Becoming proficient in this skill allows her to participate in her healthcare and wellness activities in a more informed manner and can also empower her to better advocate for herself.
Fertility awareness charting is truly one of the most valuable skills a woman can learn, and the body literacy that comes with it lasts a lifetime.
Looking for more resources?
If you want to learn more about tracking your own cycle, so that you can harness this powerful health tool and/or manage your fertility, I invite you to visit my website. I have a variety of courses available depending on the level of knowledge and support you’re looking for. I also offer complimentary, 30-minute connection calls here to help you figure out which method of fertility awareness best suits your needs, lifestyles, and preferences. For an in-depth conversation and comparison of the FEMM and Billings Ovulation Method teacher training programs, feel free to schedule a 1-hour consultation.

About the Author
Brittany Bair, FAE, IC-FHS
Brittany is a fertility awareness educator, certified to teach both FEMM and the Billings Ovulation Method. She is also a graduate of the IAFHH Functional Hormone Specialist Certification Program. Brittany currently teaches online in 1:1 live calls and occasional group sessions. She has taught women in a variety of reproductive situations how to effectively avoid pregnancy using fertility awareness – including women who are postpartum and breastfeeding, or those who have recently discontinued hormonal birth control. Brittany has a particular interest in charting for health purposes and will be releasing a comprehensive digital course (with live instructor follow-up) in 2023. The course will cover fertility awareness charting to avoid pregnancy as well as a wealth of hormone health and wellness information.
Want to showcase your expertise & business as a guest author for the IAFHH Publication?
You can contact us here or send us an email at info@iafhh.com with your inquiry and we will get back to you regarding options and opportunities for being featured in the next IAFHH Publication.
